Autoimmune diseases are a group of disorders characterized by the immune system attacking the body’s own cells and tissues.
These conditions, including lupus, rheumatoid arthritis, and multiple sclerosis, affect millions of individuals worldwide.
Notably, women are disproportionately affected by autoimmune diseases compared to men, with approximately 80% of patients being female.
The underlying reasons for this gender disparity have long puzzled scientists. However, recent research conducted by Stanford University sheds new light on this phenomenon, offering insights into the role of the X chromosome in autoimmune disorders.
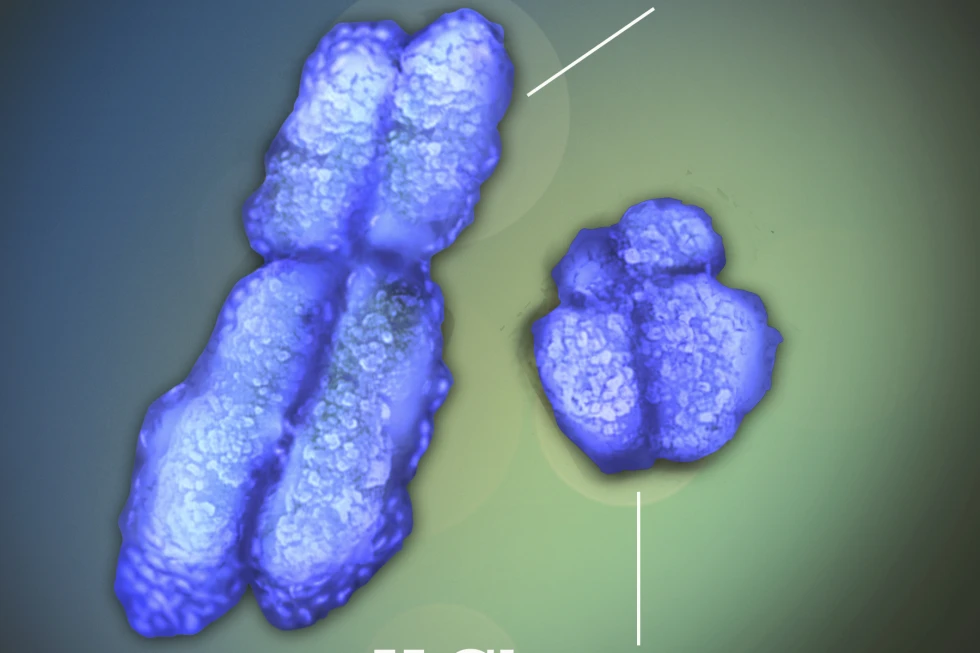
The human genome consists of 23 pairs of chromosomes, including the sex chromosomes that determine an individual’s biological sex. Females possess two X chromosomes, while males have one X and one Y chromosome.
This fundamental genetic difference has been hypothesized to contribute to the increased susceptibility of women to autoimmune diseases.
The recent study published in the journal Cell delves into the intricate mechanisms through which the X chromosome influences autoimmunity.
A pivotal discovery from the Stanford University research is the involvement of the X chromosome in a previously unforeseen manner.
The process of X-chromosome inactivation, crucial for females to regulate gene expression from the additional X chromosome, is mediated by a specialized type of RNA known as Xist.
This long RNA molecule plays a pivotal role in silencing one of the X chromosome copies in each female cell, preventing the toxic effects of an excessive gene dosage
The study reveals that abnormalities in the X-chromosome inactivation process, particularly dysregulation of Xist-mediated silencing, may underlie the heightened autoimmune susceptibility observed in women.
By elucidating the intricate molecular mechanisms governing X-chromosome inactivation, the research provides a compelling explanation for the male-female bias in autoimmune diseases.
Furthermore, the insights gained from this research may pave the way for personalized approaches to managing autoimmune diseases, taking into account the unique genetic and molecular characteristics of each patient.
By leveraging the knowledge of X-chromosome involvement in autoimmunity, clinicians and researchers can strive towards more effective, tailored treatments that address the specific underlying mechanisms driving disease pathogenesis in individual patients.
Dr. Howard Chang, a dermatologist at Stanford University, was delving into the intricacies of how Xist functions when his laboratory uncovered nearly 100 proteins that are associated with this particular molecule.
Upon further examination, Chang and his team discovered that many of these proteins are linked to autoimmune disorders related to the skin, where patients develop autoantibodies that erroneously attack these normal proteins.
This revelation led Chang to ponder on the possibility that Xist, a molecule exclusively found in women, could potentially organize proteins in a way that activates the immune system.
However, it is important to note that Xist alone cannot be the sole cause of autoimmune diseases, as not all women are affected.
Scientists have long believed that a combination of genetic susceptibility and environmental triggers, such as infections or injuries, are necessary for the immune system to malfunction.
For instance, the Epstein-Barr virus has been linked to multiple sclerosis. In an effort to further understand the role of Xist, Chang’s team engineered male lab mice to artificially produce Xist without silencing their only X chromosome, and observed the effects.
Additionally, they bred mice that are predisposed to a lupus-like condition, which can be induced by a chemical irritant.
This research opens up new avenues for exploring the complex interplay between genetics, environment, and immune system function in the development of autoimmune diseases.
The study conducted by the team revealed that the mice that produced Xist formed its hallmark protein clumps and, when triggered, developed lupus-like autoimmunity at levels similar to females.
This discovery is of great significance as it suggests that Xist RNA leaking out of the cell is crucial for the immune system to recognize it.
The environmental trigger plays a key role in initiating the autoimmune response. The research also extended to human subjects, with blood samples from 100 patients showing autoantibodies targeting Xist-associated proteins that were previously not linked to autoimmune disorders.
This suggests that standard tests for autoimmunity using male cells may have overlooked important factors.
While further research is needed, these findings have the potential to streamline the diagnosis of patients with diverse clinical and immunological presentations.
Understanding the larger Xist complex could provide a clearer picture of disease patterns and lead to more effective treatment strategies.
This study represents a significant step towards unraveling the complex biological context of autoimmune disorders.

In conclusion, the groundbreaking research from Stanford University offers a paradigm-shifting perspective on the male-female bias in autoimmune diseases.
By elucidating the intricate role of the X chromosome, particularly the process of X-chromosome inactivation mediated by Xist, the study provides a compelling explanation for the heightened susceptibility of women to autoimmune disorders.
This newfound understanding not only sheds light on a long-standing mystery in the field of immunology but also holds immense promise for advancing the diagnosis and treatment of autoimmune diseases.
As we continue to unravel the complexities of the human genome and its impact on health and disease, the insights gleaned from this research mark a significant step forward in our quest to combat autoimmune disorders and improve the lives of millions affected by these debilitating conditions